By Scihealthhub – December 4, 2024
Pressure sores, also known as bedsores or pressure ulcers, progress through four (4) stages, each marked by increasing severity and damage to the skin and underlying tissues.
Individuals with limited mobility, such as those with spinal cord injuries, who spend extended periods sitting or lying down, are at the highest risk of developing pressure sores.
Prolonged sitting or lying causes sustained pressure on the skin and underlying tissues. This can restricts blood flow to the area, depriving tissues of oxygen and nutrients. Without adequate circulation, the affected tissue can become damaged and eventually die, leading to the formation of sores
Between 50% and 80% of people with spinal cord injuries experience at least one pressure sore during their lifetime (1).
Common sites for pressure sores include bony prominences such as the buttocks, hips, elbows, heels, tailbone, lower back, and shoulder blades.
Understanding the four stages of pressure sores is imperative for early detection and effective management.
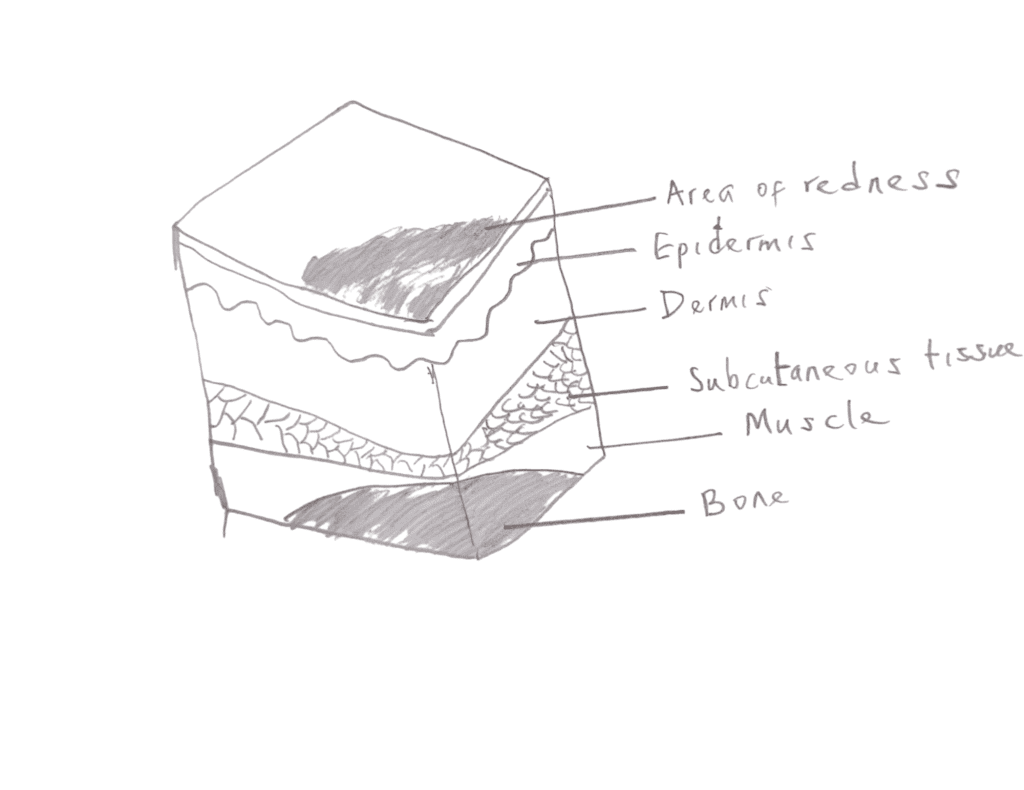
Stage 1: Non-Blanchable Redness of Intact Skin
Characteristics:
- The skin remains intact but shows persistent redness that does not fade when pressed (non-blanchable). In people with darker skin tones, this redness may be harder to detect.
- Affected areas may feel harder, warmer than surrounding skin, or swollen.
- Symptoms may include pain, tenderness, itching, or discomfort in the area.
Steps to Take:
1. Relieve pressure from the affected area immediately by repositioning regularly.
2. Use specialized cushions, mattresses, or padding to reduce pressure.
3. Keep the skin clean, dry, and well-moisturized.
4. Ensure adequate hydration and nutrition to support skin health.
5. Consult a doctor if there is no noticeable improvement within 2–3 days.
You might also like to see How I Survived a Pressure Sore Scare
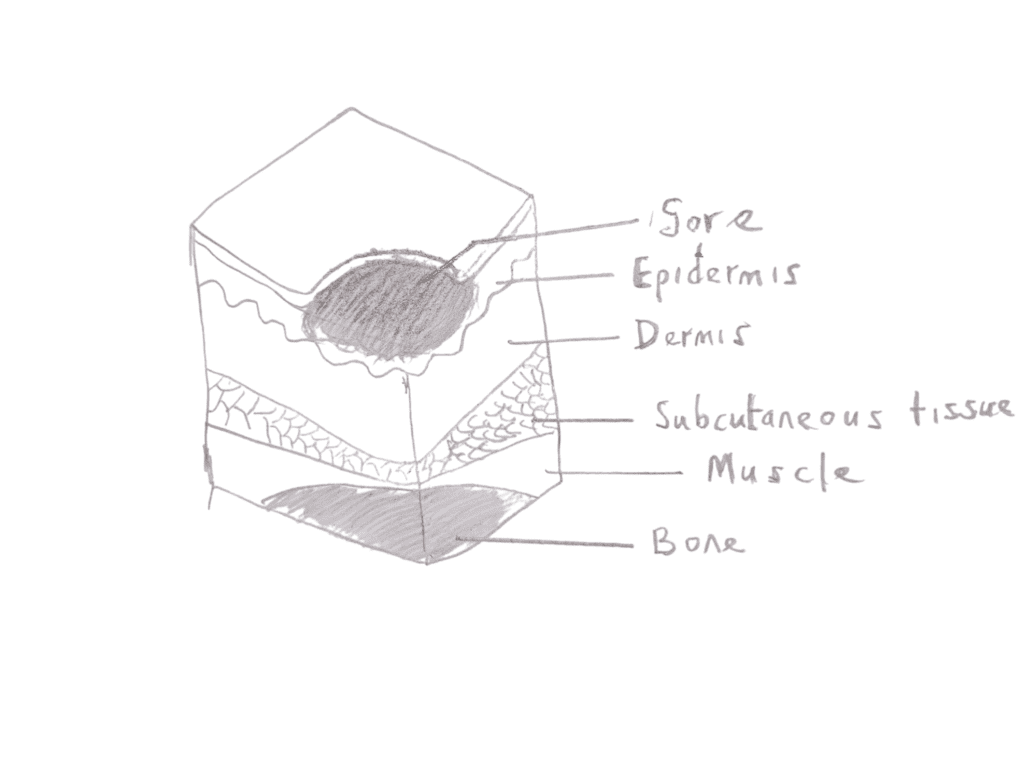
Stage 2: Partial-Thickness Skin Loss
Characteristics:
- The outermost skin layer (epidermis) and sometimes part of the dermis are damaged, resulting in a shallow open wound.
- The wound may appear as an open blister, abrasion, or shallow crater.
- It may ooze clear or yellowish fluid, indicating tissue damage without deep tissue involvement.
Steps to Take:
1. Continue pressure relief and regular repositioning.
2. Use specialized cushions, mattresses, or padding to minimize pressure.
3. Clean the wound with saline or an appropriate wound-cleaning solution.
4. Apply protective dressings, such as hydrocolloid or foam dressings, to keep the wound moist and promote healing.
5. Change the wound dressing regularly.
6. Ensure adequate hydration and nutrition to support skin repair.
7. Consult your healthcare provider if signs of infection develop, such as increased redness, swelling, or pus.
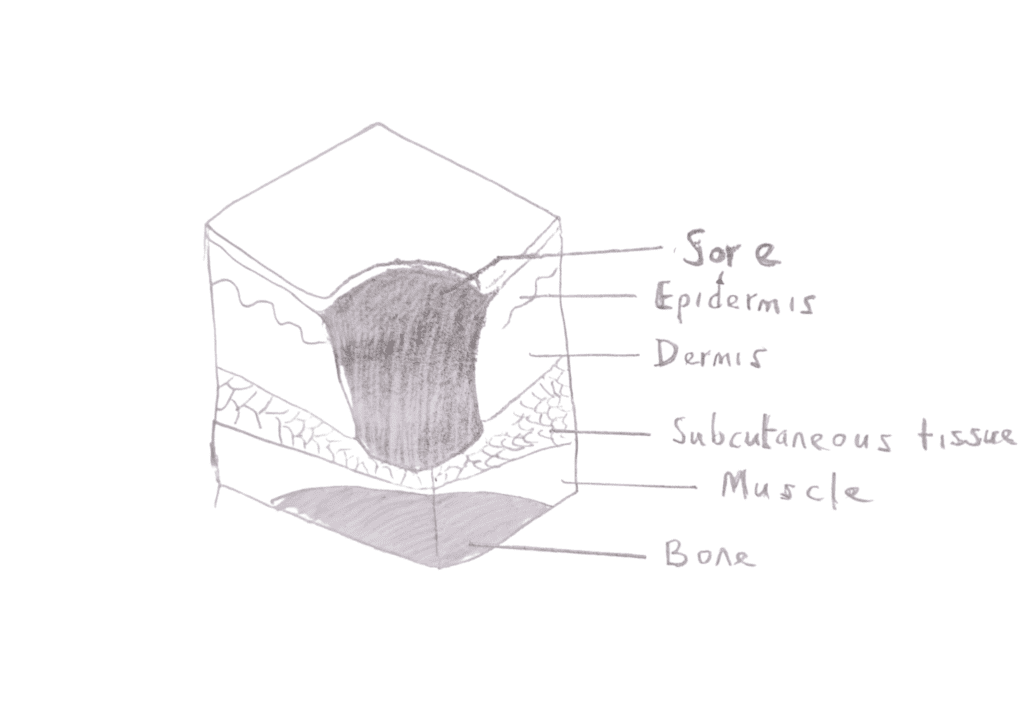
Stage 3: Full-Thickness Skin Loss
Characteristics:
- The wound extends through the two layers of skin (epidermis and dermis) into the subcutaneous tissue but does not reach the muscles, tendons, or bone.
- It may appear as a deep crater with visible fat but without exposed bone, muscle, or tendon.
- Parts of the wound may contain slough (yellowish dead tissue) or eschar (dark, scab-like tissue).
Steps to Take:
1. Continue Pressure Relief: Regularly reposition to reduce pressure on the wound.
2. Use Specialized Support: Employ pressure-relief cushions or mattresses to minimize further tissue damage.
3. Nutritional Support: Ensure an adequate intake of protein, vitamins (especially vitamin C), and zinc to promote tissue repair.
4. Medical Interventions:
- Debridement: Remove dead or infected tissue to encourage healing. This can be done surgically or with enzymatic solutions.
- Negative Pressure Wound Therapy (NPWT): Use a wound dressing system that applies continuous or intermittent suction to promote healing.
- Surgery: In some cases, surgical closure of the wound may be necessary.
5. Pain Management: Use appropriate painkillers to relieve discomfort.
6. Seek Medical Attention: Contact a healthcare provider promptly if you experience signs of systemic infection or worsening wound conditions, such as:
- Fever
- Increased redness, pain, or swelling
- Foul odor or excessive drainage
- Darkening or discoloration of the wound edges
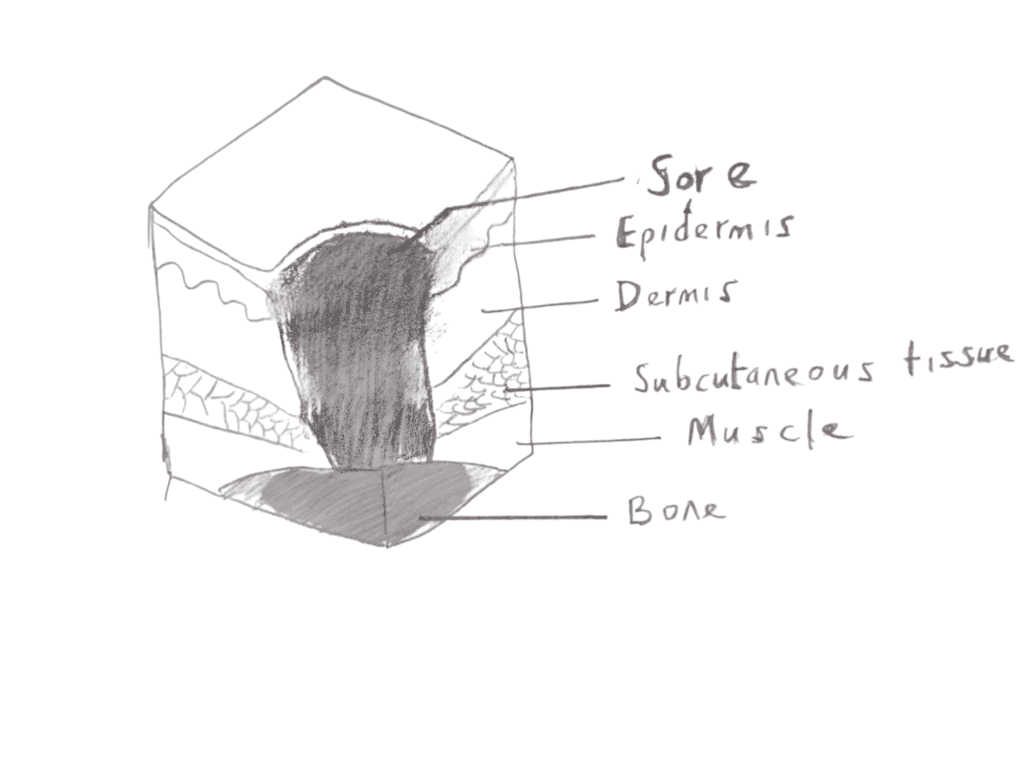
Stage 4: Full-Thickness Tissue Loss with Exposed Bone, Muscle, or Tendon
Characteristics:
- The wound extends through all layers of skin into the muscle and may expose bone, tendons, or joints.
- Significant amounts of dead tissue and drainage are typically present.
- These sores are highly prone to infection, including osteomyelitis (bone infection) or sepsis.
Steps to Take:
1. Seek Immediate Medical Intervention: Prompt treatment is essential to prevent life-threatening complications.
2. Surgical Debridement: Removal of dead tissue is typically necessary to reduce infection risk and promote healing.
3. Advanced Wound Care Therapies:
- Negative Pressure Wound Therapy (NPWT): Uses suction to enhance healing.
- Hyperbaric Oxygen Therapy: Delivers oxygen to the wound to accelerate tissue repair.
4. Surgical Intervention: Procedures like skin grafts or flap surgery are often needed to close the wound.
5. Systemic Antibiotic Therapy: Due to the high risk of infection, antibiotics are often required.
6. Aggressive Pressure Relief: Continue frequent repositioning to alleviate pressure.
7. Specialized Support Surfaces: Use pressure-relief cushions or mattresses to protect the affected area.
8. Pain Management: Administer appropriate pain relievers for comfort.
9. Nutritional Support: Ensure adequate intake of protein, vitamins (especially vitamin C), and zinc to support tissue repair.
Conclusion:
Pressure sores are serious, potentially life-threatening complications, especially for individuals with limited mobility. Understanding the four stages and implementing proactive measures can help individuals and caregivers effectively manage and reduce the risk of pressure sores.